Executive Summary
While overall health workforce shortages persist, some professions are growing rapidly. The supplies of nurse practitioners (NPs) and physician associates (PAs) are projected to increase by 66% and 37%, respectively, between 2024 and 2034.1 Both professions have historically been seen as vital to expanding access to primary care services and care for rural populations.
Some policymakers have suggested that demand for physician services will be met as patients are treated by NPs and PAs in a physician scarce environment. Others have expressed concerns as surpluses of NPs and PAs are projected in federal workforce models. More and better information is needed on the roles and contributions of NPs and PAs on the care team to understand how this might play out and to facilitate policies to better ensure timely access to high-quality care.
This paper presents an approach to better understanding the roles and contributions of NPs and PAs on the care team. As the evidence base grows, this new knowledge should be incorporated into existing workforce projections models.
As health workforce projections models are improved with new information on the different roles of NPs, PAs, and other members of the care team and different team configurations, policy conversations that acknowledge the current complexities of care provision and devise realistic policy solutions to the health workforce shortages can take place at the local, state, and federal levels.
Introduction
Workforce shortages have characterized the health care delivery system for many years, dating back to at least the middle of the last century.2 The challenges and requirements of providing care to a rapidly aging population continue.3 4 5 The COVID-19 pandemic exacerbated existing shortages by increasing demand for inpatient services and requiring the rapid redeployment of workers; COVID-19 also took a toll on health care workers’ physical and mental well-being.6 7 8 9 10 As the pandemic has entered an endemic phase, the challenge of addressing workforce shortages persists. Moreover, projections of future health workforce shortages across many professions and specialties also persist.
In a previous paper on workforce projections modeling11 the AAMC Research and Action Institute identified several deficits of current projections models, including that many projections focus on a single profession or occupation. That is, a profession or specialty is often considered in a vacuum, as if it were practicing in a delivery system isolated from all other professions and occupations that also provide care for patients. At times, workforce projections have also optimistically assumed that patients would appropriately present to an idealized provider for their chief complaint or condition without evidence that individuals behave in this fashion.
Models that assume a significant change in patient (and provider) behavior should be viewed with skepticism.
The reality is that health care is provided in much more interconnected (and often disorganized) ways, with many professions and occupations playing roles and working together (or in parallel) to deliver care to patients (refer to Table 1). Without accounting for the interconnectedness of care, projections of future health workforce supply and demand, and policy informed by them, will inevitably be limited. Projections that fix current practice patterns in the future and projections based upon policy and practice states that are wished for but unlikely in the near term (e.g., assuming all patients will perfectly present to the member of the team in every setting best equipped to care for them, with seamless transitions between sites and providers) are also of limited utility. Care continues to evolve, and projections models and policy need to do the same.
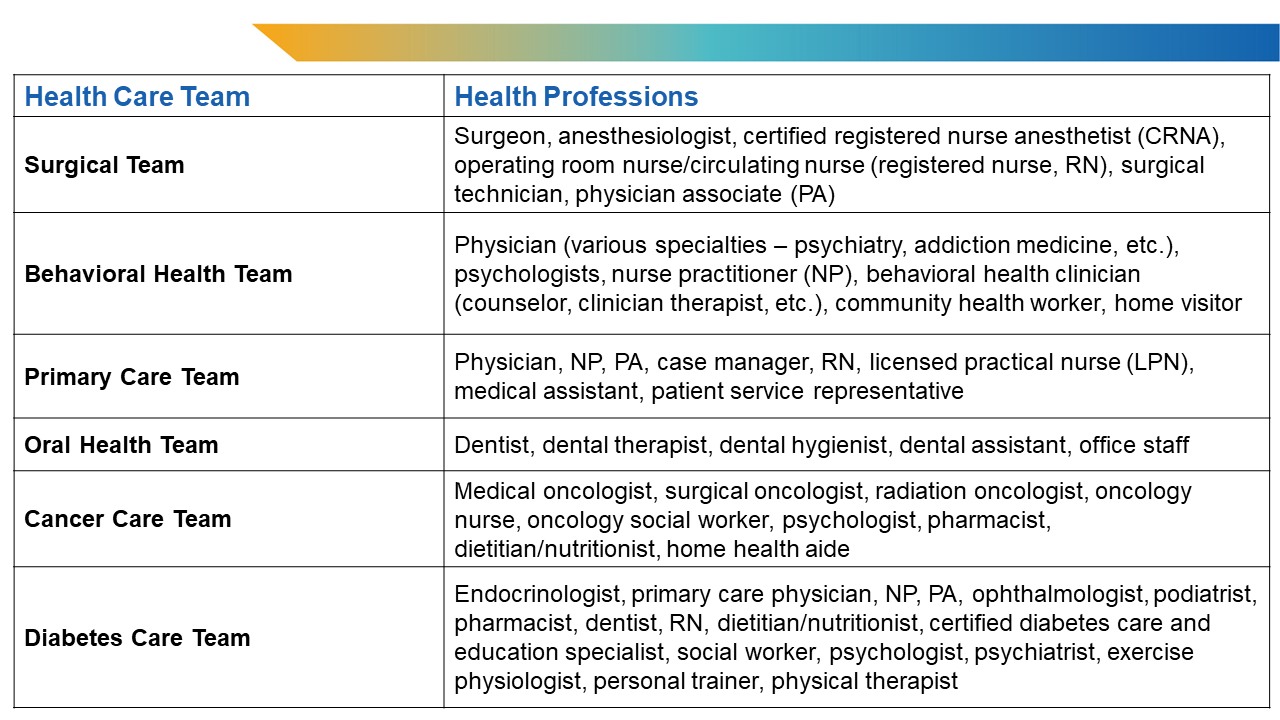
Table 1. Examples of Care Teams and Their Members.
In this paper, I suggest a two-part strategy to approach this data and analytic deficit and outline the beginnings of a new framework that accounts for the reality of current and future practice to address current and projected health workforce shortages. To illustrate the problem and strategy, I consider the case of nurse practitioners (NPs) and physician associates (PAs), two professions that have experienced tremendous growth over the past decade.12 13
In recent projections of primary care supply, some models suggest both surpluses of NPs and PAs and shortages of family physicians and general internists.14 This scenario is unlikely to occur for several reasons. Patients may satisfy their unmet demand through new entry points to care (other professionals); providers in certain specialties or geographic locations that find themselves in limited demand in response to a surplus of clinicians may change their practice; or the projections themselves might not adequately capture how care is provided and the contributions of different care team members, including the broadening of services offered in a particular office, clinic, or geography. Projections that incorporate realistic, improved approaches to clinical practice can help avoid historically unlikely projections of large numbers of providers being in surplus while others are in shortage when they potentially care for similar patients.
Ideally, data to inform projections would be based not just upon the health care professional providing services, but on the behavior, characteristics (personal as well as social determinants of health), and conditions of the patients who are seeking (or choosing not to seek) care and might present in a variety of settings to a number of different providers. To better understand these patterns, it is useful to step back and examine the history and practice patterns of other clinicians, starting with NPs and PAs.
Origins of NPs and PAs
Nurse practitioners are licensed health care providers who practice in every specialty and setting. NPs originated in the mid-1960s with the establishment of the first educational program at the University of Colorado by Loretta Ford, EdD, and Henry Silver, MD, to improve local access to primary care services.15 16 Over time, as the number of NPs grew and the profession became more established, NPs became important contributors to primary and specialty care across the health care delivery system. However, since the beginning of the profession, the quality of care (and scope of practice) provided by NPs has been questioned by physicians. This has led to variability in practice authorization across states. The NP profession has worked to increase the practice authority of NPs based on research on health outcomes and safety of care provided by NPs.17 As of March 2023, NPs have full, independent practice authority in 27 states.18 19
Physician associates are also licensed by the state and practice in every specialty and setting. Like NPs, PAs also originated in the mid-1960s with the establishment of the first physician assistant educational programs at Duke University by Eugene Stead, MD, in 196520 and the MEDEX program at the University of Washington by Richard Smith, MD.21 Similar to NPs, PAs originated as a response to primary care shortages. The initial educational programs trained former military corpsmen to become PAs.22 PAs, too, have become important contributors to both primary care and specialty care in the United States. PA scope of practice — and specialty — is determined, with some variation across states, at the institution, system, or practice level according to the needs of the patients and the education, experience, and preferences of the care team.23 Expanding autonomy and standing relative to physicians and other practitioners has been important to the PA profession. For example, recently, the profession changed its title from “physician assistant” to “physician associate” to better position itself to compete in the health care delivery marketplace.24
Supply and Demand for NPs and PAs Has Grown Dramatically
Both NP and PA workforces have grown rapidly over the past decade. Data from the Bureau of Labor Statistics indicate that the number of employed NPs has more than doubled since 2011 and the number of employed PAs has increased by almost 50% during that time period (Figure 1). At the same time, the production of new NPs and PAs has also dramatically increased (Figure 2). Relative to physicians, NPs and PAs have shorter educational tracks and training programs and therefore their workforces can expand more quickly.25 These trends have led to projections of continued growth in the national supply of NPs and PAs for the foreseeable future, with NP supply growing by 66% and PA supply growing by 37% between 2024 and 2034.26
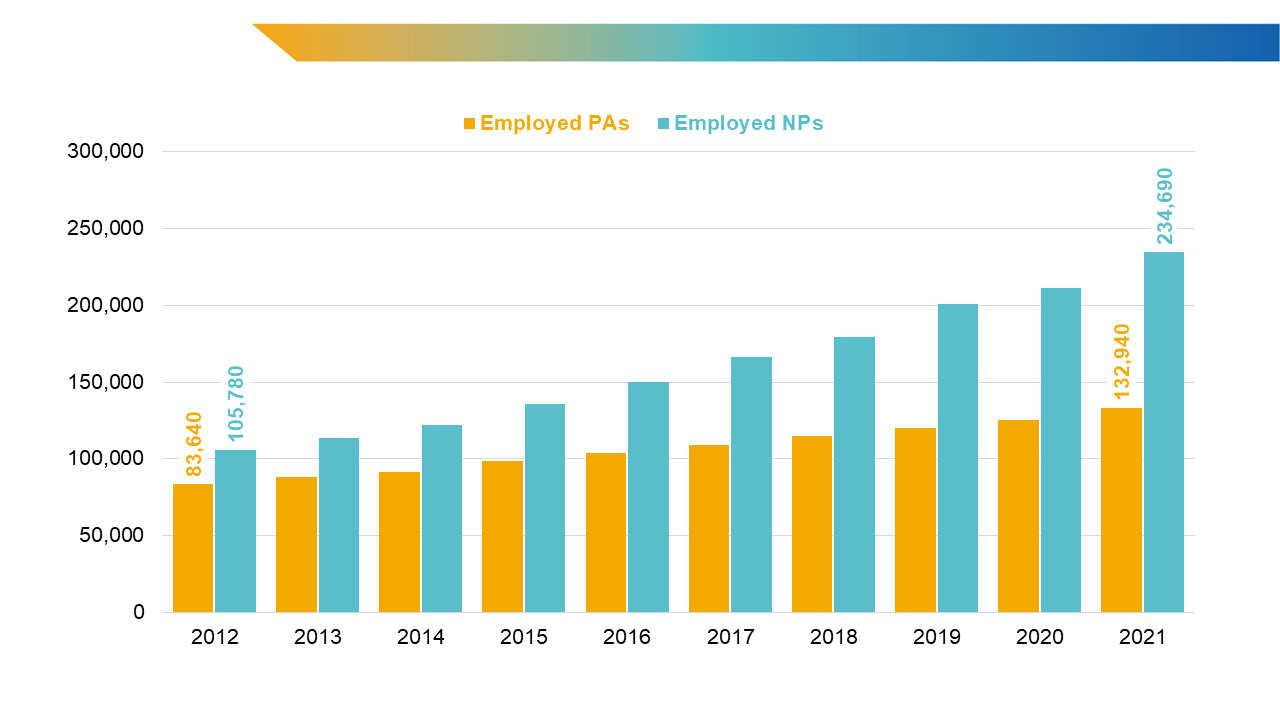
Figure 1. Growth in employed PAs and NPs, 2012-2021.
Sources: Bureau of Labor Statistics. National Occupational Employment and Wage Estimates, May 2012-May 2021. Accessed July 20, 2023. https://www.bls.gov/oes/
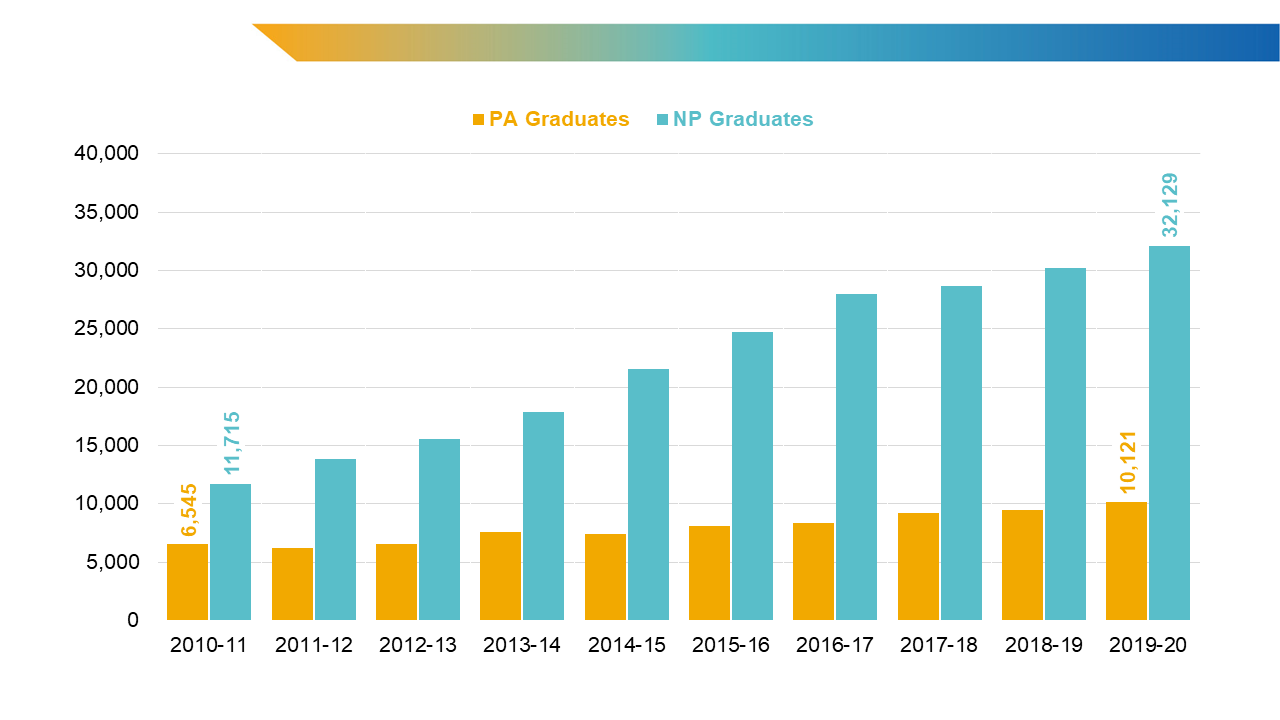
Figure 2. Growth in PA and NP graduates, 2010-2020.
Sources: PA Education Association. Annual reports, 2012-2019. Accessed July 20, 2023. https://paeaonline.org/resources/public-%20resources/research-reports/program-survey-and-reports ; Hooker RS, Cawley JF. Physician assistants/associates at 6 decades. Am J Manag Care. 2021;27(11):498-504. doi:10.37765/ajmc.2021.88777 ; Salsberg E. Changes in the Pipeline of New NPs and RNs: Implications for Health Care Delivery and Educational Capacity. Health Affairs Blog. Published 2018. doi:10.1377/hblog20180524.993081; American Association of Colleges of Nursing. Enrollment and Graduations in Baccalaureate and Graduate Programs in Nursing reports, 2018-2019, 2019-2020, and 2020-2021. s
Primary care and other physician shortages have persisted and, as costs have grown, health systems and policymakers alike have looked to other health professionals to provide care at a lower cost than physicians. Team-based approaches to care have grown, and the roles of NPs and PAs on the care team (and other care models) have expanded. Working alongside (or in parallel to) physicians and other clinicians, NPs and PAs provide care to patients in all specialties and settings. As their roles have expanded, NPs and PAs have become increasingly important contributors by improving access to care in rural areas and designated Health Professional Shortage Areas. NPs and PAs have been shown to provide equivalent quality and cost-effective care relative to physicians in several contexts, including primary care, chronic disease management, and specialty care, and in community health centers and other contexts.27 28 29 30 Moreover, newer models of care such as accountable care organizations, patient-centered medical homes, and other integrated care models, characterized by more delegation of work, new technologies, streamlined care processes, and potential cost savings, have created more opportunities for NPs and PAs.31 32
Some projections of demand for NPs and PAs indicate growth of approximately 9% from 2024 through 2034.33 Other projections suggest more robust demand growth — 38% for NPs and 27% for PAs between 2022 and 2032.34 35 But there are no projections of demand for either of these professions near those for their supply growth. Under most current models, baseline projections of adequacy of the NP and PA workforces indicate excess NPs (as high as 78% more than demand) and PAs (as high as 26% more than demand) in 2034.36 These projections have led some to suggest that there will be a large surplus of NPs and PAs in the near future.37 38 Moreover, some have expressed concerns about the implications of the potential surplus for other professions, specifically in terms of exacerbating existing shortages of registered nurses.39 40 At the same time, these projections become difficult to reconcile with unemployment rates among NPs and PAs hovering around 1%.41 42 43
The Problem
The potential mismatch in supply and demand in primary care described above is due partly to projections models’ inability to capture the interconnectedness of how care is provided to patients. Available data used to build models do not sufficiently capture the extent to which and how care teams are being created and configured and how they are delivering care. Without better information on how care is provided and work is shared by the team, some models rely on assumptions about staffing ratios of one type of provider to another (e.g., the number of NPs or PAs to physicians) in order to extrapolate demand for different kinds of providers.44 This strategy leads to the reduction of a provider’s contribution to some percentage or proportion of another type of provider, usually a physician, and arguments about efforts to replace physicians with other types of providers. Moreover, such assumptions (where an NP’s or PA’s contribution is equated to some percentage of a physician’s effort) presume health professionals function in silos and do not calculate the impact of how different professionals may interact within teams or across practice settings. Even within models that make these kinds of assumptions, there is limited agreement on what theoretical percentage of physician care can be delivered by others and very little data on how that care is delivered in different clinical settings and specialties.
A Potential Solution
To approach this modeling deficit, better project supply and demand for NPs and PAs, and suggest the beginnings of a new framework for addressing workforce analyses, I propose a two-pronged strategy.
The first part of this strategy is finding and analyzing relevant data on the contributions of NPs and PAs in team settings and in independent settings. As team-based care has become more desirable, especially in the transition from volume- to value-based care models, its impact should be better studied. While research suggests that team-based care may improve the safety, quality, and efficiency of care delivery, the patient experience of care, and clinician wellness,45 46 47 48 49 50 questions remain. Data collection should include information about how workload is shared across professionals in isolation or in teams, in one clinic or across locations (including virtual settings). The questions about NPs and PAs to be addressed might start with:
- What conditions do they treat?
- What spectrum of care do they provide?
- Which patients do they care for?
- How do these patients vary by complexity and medical condition?
- How do tasks vary by provider type and level of experience or proximity to/collaboration with other clinicians?
- How do NP and PA contributions relate to physician (and other members of the care team’s) contributions?
- What is the degree of interdependence among members of the care team?
- What roles do practice culture, financing model, and other practice characteristics play?
Another layer of analysis would examine how the contributions of NPs and PAs vary given other contextual factors, such as characteristics of the practice environment, including types of practices in the local market, demographic characteristics and socioeconomic status of the local population, and prevalence of different types of providers.
Data to inform these sorts of analyses and describe how the care workload is shared, while not publicly available, might be found in electronic health record systems, especially in well-organized health systems that are already monitoring provider workloads and utilization and claims records. Care needs to be taken with the latter, however, as the accuracy of who provides care compared to how the care is billed to the payer (e.g., incident-to billing) has been questioned; there are concerns that such billing practices underestimate of the contributions of NPs and PAs and overestimate of the contributions of physicians.51 52 53
To be sure, work like this is already occurring in the study of primary care teams.54 55 56 As the evidence base grows, it should be incorporated into workforce projections models.
The second part of this strategy is reframing workforce practice and policy parameters to reflect reality while allowing for creative scenario planning. As the analyses above are being conducted and their findings integrated into workforce projections models, it is important to reframe several workforce policy parameters to develop policy that better addresses current and projected workforce shortages.
First, workforce policy should recognize the care team in its current state. As discussed previously, single-profession-focused analyses, projections, and policy have been the norm. But care has evolved, and policy needs to catch up to the realities of practice while ensuring quality care for patients. Even when NPs, PAs, and other providers practice independently, patients flow between them. In some cases, other providers offer an alternate and more convenient entry point into care; in others, care is specifically and intentionally shared between providers who work together. If the goal is to have more of the latter model, how do we create feasible policies at the state and federal levels to move from a fragmented approach to a more integrated and efficient one? Understanding this stepwise transition with periodic assessment and integration of practice data into evolving models will be required to project need, demand, and supply of health services with greater accuracy and relevance.
How planners, researchers, or policymakers desire the system to operate then has to be tempered with reality of how long changes in workforce supply and practice patterns take to achieve. Much of the focus in addressing health workforce shortages has been centered around physicians, but physicians take many years to educate and train. Alternatives such as relying on already trained physicians and other providers from abroad generate their own set of problems.57 58 Modifying the care team, especially if applying actual current models of care, may hasten the relief of workforce shortages and improve the quality of care. However, models must also account for the continuum of current practice at the local level, from clinicians working in well-organized integrated teams to clinicians working in a more isolated manner.
Second, workforce research and policy should focus on patients’ needs and desires and ensuring that these are met. The change in focus requires moving away from thinking solely about shortages of physicians and committing to the idea of care delivered by a variety of health professionals, sometimes in teams, sometimes in isolation. Team members can and do have overlapping scopes of practice and could adapt depending on patients’ needs and on the professional makeup, experience, and organization of the care team.59 60 But for care to be delivered in teams also requires attention to patient behavior and choice. The policy goal must move from solely matching a single type of provider in existing or theoretical models to the realistic delivery of effective, quality services in health care. Such a focus will foster flexibility and innovation with regard to care models and policy.61 62
Examples of innovative team-based models of care tied to the needs of patients include integrating behavioral and oral health care in primary care service delivery,63 64 65 diabetes care and management,66 Learning from Effective Practices (LEAP) program primary care practices,67 68 and others in academic medical centers69 and hospitals and health systems. In addition, as mentioned above, as part of the suggested reframing, policy should refrain from reducing a provider’s contribution to some percentage or proportion of another type of provider. Instead, policy should focus on the services the team can provide effectively and how members contribute. Ideally, any policies should identify the current needs of populations. These policies must acknowledge the realities of existing practice patterns, the potential “unnecessary” services policymakers wish to eliminate, and the services that populations desire or need that are not currently delivered or are delivered ineffectively, inequitably, or inefficiently. Projections must also include realistic time frames for modeling changes in practice delivery scenarios.
Policy will also need to effectively navigate overlapping scopes of practice and be flexible enough to support local needs and practices and care delivery innovation.70 Policy should also, however, recognize the potential tensions among efforts to address health workforce shortages amid established professional hierarchies and scopes of practice.71
Finally, workforce policy should be based on evidence and actual experience rather than simply the end goal of a particular theorized state of care. This point brings the strategy full circle, as the starting point for both policy and health workforce projections modeling becomes grounded in what is actually happening in the health care delivery world.
Opportunities and Barriers
Implementing the strategy outlined above will take some time. The implied steps in the data prong — identifying the data, entering into the appropriate partnerships with the data stewards to obtain and use the data, analyzing the data, turning over the results of the analyses to projections modelers to integrate into their models, and generating improved health workforce projections for NPs, PAs, and physicians — will not happen overnight. So, what can be done now? Recently, several health workforce researchers advocated for modernizing scope-of-practice regulation.72 This action requires a better understanding of current delivery patterns and the openness of practitioners and policymakers to change. Importantly, part of their suggestion involved providers engaging with provider associations, health system leaders, and policymakers to describe their experiences providing care using innovative models, demonstrate where their efforts to change have met barriers, and discuss whether and when these barriers are likely to change.
Likewise, as work along the data prong is commencing, it will be critical to engage the key stakeholders, including physicians, NPs and PAs, their representative associations, health system leaders, policymakers, projections modelers, and other workforce research experts, in thinking about how NPs, PAs, and physicians share the work of providing care to patients. A key focus of this initial engagement should be understanding what NP, PA, and physician roles are currently, what they might be in the near term, and what they are ideally in the long term.
In the course of that engagement, two important goals can be accomplished. First, stakeholders can lay the groundwork as they wait for the data and projections models catch up. That might include reorienting the policy focus from the individual provider to the patient and the team required for the improved data and projections models to be useful in developing future workforce policy. Second, stakeholders can develop and negotiate near-term local solutions to organize and deploy a health workforce that best meets the needs of patients and relieves workforce shortages. Even then, getting from the current state of practice to the “ideal” state requires removing barriers and establishing the conditions needed to achieve change.
As suggested in a prior paper, improving the availability of data to help understand how NPs, PAs, physicians, and others on the care team interact is vital to improving the projections models and making them more useful to policy- and decision-makers. Currently, these data are not readily available. They exist in private health systems and are generally not available to researchers or those who develop projections models. In fact, some have argued that the data that are available publicly in Medicare claims and expenditure files underestimate the contributions of the care team73 74 75 ; yet these data often underestimate the role of providers who are not physicians because of the financial incentives for billing through a physician even when they are only peripherally relevant to care. Revisions to Medicare claims and expenditure files to ameliorate the errors leading to misattribution of NP and PA contributions to care provided would be an important step to reduce the effect of this barrier.
Final Thoughts
Understanding the contributions of NPs and PAs to patient care from independent practice to a team environment is vital to improving workforce projections models. It is one of the first steps to better grounding these models, and therefore the projections they generate, in how care is provided to patients. While current projections of NPs and PAs suggest a likely oversupply of these providers in primary care and a simultaneous shortage of primary care physicians in the future, it is impossible to interpret the implications of those projections without incorporating a better understanding of how NPs and PAs contribute to care for patients and share these responsibilities with physicians and others.
Better defining the current breadth of NP and PA contributions to care can also inform how care is delivered by other professionals such as pharmacists, social workers, therapists, and others. Workforce projections models should adapt to how the workforce changes, including how it is composed, how it is deployed, and how it accomplishes its work. As the workforce changes, so should models that represent it. Workforce projections models informed with a better understanding of how all members of the care team contribute to care would greatly improve the usefulness of these models for policy. Devising and evaluating potential strategies to forestall future projected workforce shortfalls require improved projections models. Projections models should also be flexible enough to examine how care might be ideally organized while acknowledging the major changes necessary to transform care delivery.
Improved projections models alone, however, are not enough to improve population health, enhance the care experience, reduce costs, improve clinician wellness, and achieve health equity (i.e., to achieve the goals of the quintuple aim).76 77 78 An important part of making progress toward these system improvement goals is understanding how specific workforce policies are linked to changes in care delivery and the behavior of both health professionals and patients. I have suggested a reoriented workforce policy that acknowledges the care team, is zeroed in on patients’ needs, and is based on evidence and experience and provided some initial steps to move forward.
Any significant changes in how the United States decides to configure, plan, and deploy its health workforce will need to acknowledge the realities of the complexities of care. Further, understanding how a desired target state may be facilitated or impeded by the current and historical realities of care delivery needs to be acknowledged as well. Barriers may include resistance from physicians regarding new models of care, team configurations, or decision-making tools. Facilitators may include the desire of health systems to further integrate to improve coordination of care and reduce costs through interprofessional teams. By better capturing and supporting the variety of care provided by different health professions, policymakers and individual health systems can move toward reoriented workforce policy that fosters a better connected, more efficient, and higher-quality health care ecosystem.
- National Center for Health Workforce Analysis. Workforce Projections. Accessed April 1, 2024. https://data.hrsa.gov/topics/health-workforce/workforce-projections Back to text ↑
- Ricketts TC. Building an Effective and Sustainable Health Care Workforce (1960s-Present). In: Oliver TR, ed. Guide to U.S. Health and Health Care Policy. 1st ed. CQ Press; 2014:197-212. Back to text ↑
- Center for Health Workforce Studies. The Impact of the Aging Population on the Health Workforce in the United States. 2005. https://www.chwsny.org/wp-content/uploads/2015/09/ImpactofAging2005.pdf Back to text ↑
- Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. The National Academies Press; 2008. doi:10.17226/12089 Back to text ↑
- Foley KT, Luz CC. Retooling the health care workforce for an aging America: a current perspective. Gerontologist. 2021;61(4):487-496. doi:10.1093/geront/gnaa163 Back to text ↑
- Impact of the COVID-19 Pandemic on the Hospital and Outpatient Clinician Workforce: Challenges and Policy Responses. Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. May 2022. https://aspe.hhs.gov/reports/covid-19-health-care-workforc Back to text ↑
- Mehta S, Machado F, Kwizera A, et al. COVID-19: a heavy toll on health-care workers. Lancet Respir Med. 2021;9(3):226-228. doi:10.1016/S2213-2600(21)00068-0 Back to text ↑
- Song YK, Mantri S, Lawson JM, Berger EJ, Koenig HG. Morally injurious experiences and emotions of health care professionals during the COVID-19 pandemic before vaccine availability. JAMA Network Open. 2021;4(11):e2136150. doi:10.1001/jamanetworkopen.2021.36150 Back to text ↑
- Chemali S, Mari-Sáez A, El Bcheraoui C, Weishaar H. Health care workers’ experiences during the COVID-19 pandemic: a scoping review. Hum Resour Health. 2022;20(1):27. doi:10.1186/s12960-022-00724-1 Back to text ↑
- Oster N, Skillman S, Frogner B. COVID-19’s Effect on the Employment Status of Health Care Workers. 2021. https://familymedicine.uw.edu/chws/wp-content/uploads/sites/5/2021/05/Health_Employ_Status_PB_May_26_2021.pdf Back to text ↑
- Forte G. Why Health Workforce Projections Are Worth Doing. Published online June 2023. doi:10.15766/rai_5xorzcnu Back to text ↑
- Auerbach DI, Buerhaus PI, Staiger DO. Implications of the rapid growth of the nurse practitioner workforce in the US. Health Aff (Millwood). 2020;39(2):273-279. doi:10.1377/hlthaff.2019.00686 Back to text ↑
- Hooker RS, Cawley JF. Physician assistants/associates at 6 decades. Am J Manag Care. 2021;27(11):498-504. doi:10.37765/ajmc.2021.88777 Back to text ↑
- National Center for Health Workforce Analysis. Workforce Projections. Accessed April 1, 2024. https://data.hrsa.gov/topics/health-workforce/workforce-projections Back to text ↑
- Brennan C. Tracing the history of the nurse practitioner profession in 2020, the year of the nurse. J Pediatr Health Care. 2020;34(2):83-84. doi:10.1016/j.pedhc.2019.12.005 Back to text ↑
- American Association of Nurse Practitioners. Historical Timeline. Accessed March 24, 2023. https://www.aanp.org/about/about-the-american-association-of-nurse-practitioners-aanp/historical-timeline Back to text ↑
- American Association of Nurse Practitioners. Issues at a Glance: Full Practice Authority. American Association of Nurse Practitioners. Published March 2023. Accessed September 5, 2023. https://www.aanp.org/advocacy/advocacy-resource/policy-briefs/issues-full-practice-brief Back to text ↑
- American Association of Nurse Practitioners. State Practice Environment. Accessed March 24, 2023. https://www.aanp.org/advocacy/state/state-practice-environment Back to text ↑
- NurseJournal Staff. Nurse Practitioner Practice Authority: A State-by-State Guide. Published March 3, 2022. Accessed March 24, 2023. https://nursejournal.org/nurse-practitioner/np-practice-authority-by-state/ Back to text ↑
- American Academy of PAs. History of the PA Profession and the American Academy of PAs. Published 2024. Accessed March 8, 2024. https://www.aapa.org/about/history/ Back to text ↑
- American Academy of PAs. MEDEX founder Richard A. Smith, MD, on the PA concept’s path. Published 2024. Accessed March 8, 2024. https://www.aapa.org/about/history/medex-founder-richard-smith-md-pa-concepts-path/ Back to text ↑
- Physician Assistant History Society®. 1957-1970: The Formative Years. Accessed March 30, 2023. https://pahx.org/period02/ Back to text ↑
- American Academy of PAs. PA Scope of Practice. Published online September 2019. Accessed Sept. 18, 2023. https://www.aapa.org/wp-content/uploads/2017/01/Issue-brief_Scope-of-Practice_0117-1.pdf Back to text ↑
- American Academy of PAs. Rebranding the Physician Assistant Profession. AAPA. Published 2023. Accessed September 4, 2023. https://www.aapa.org/title-change/process/ Back to text ↑
- Auerbach DI, Staiger DO, Buerhaus PI. Growing ranks of advanced practice clinicians — implications for the physician workforce. N Engl J Med. 2018;378(25):2358-2360. doi:10.1056/NEJMp1801869 Back to text ↑
- National Center for Health Workforce Analysis. Workforce Projections. Accessed April 1, 2024. https://data.hrsa.gov/topics/health-workforce/workforce-projections Back to text ↑
- Kurtzman ET, Barnow BS. A comparison of nurse practitioners, physician assistants, and primary care physicians’ patterns of practice and quality of care in health centers. Med Care. 2017;55(6):615-622. doi:10.1097/MLR.0000000000000689 Back to text ↑
- Abraham CM, Norful AA, Stone PW, Poghosyan L. Cost-effectiveness of advanced practice nurses compared to physician-led care for chronic diseases: a systematic review. Nurs Econ. 2019;37(6):293-305. Back to text ↑
- Martin-Misener R, Harbman P, Donald F, et al. Cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: systematic review. BMJ Open. 2015;5(6):e007167. doi:10.1136/bmjopen-2014-007167 Back to text ↑
- Perloff J, DesRoches CM, Buerhaus P. Comparing the cost of care provided to Medicare beneficiaries assigned to primary care nurse practitioners and physicians. Health Serv Res. 2016;51(4):1407-1423. doi:10.1111/1475-6773.12425 Back to text ↑
- Hooker RS, Muchow AN. Supply of physician assistants: 2013-2026. JAAPA. 2014;27(3):39-45. doi:10.1097/01.JAA.0000443969.69352.4a Back to text ↑
- Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians. Health Aff (Millwood). 2013;32(11):1881-1886. doi:10.1377/hlthaff.2013.0234 Back to text ↑
- National Center for Health Workforce Analysis. Workforce Projections. Accessed April 1, 2024. https://data.hrsa.gov/topics/health-workforce/workforce-projections Back to text ↑
- U.S. Bureau of Labor Statistics. Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners. Occupational Outlook Handbook. Published September 6, 2023. Accessed April 1, 2024. https://www.bls.gov/ooh/healthcare/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm Back to text ↑
- U.S. Bureau of Labor Statistics. Physician Assistants. Occupational Outlook Handbook. Published September 6, 2023. Accessed April 1, 2024. https://www.bls.gov/ooh/healthcare/physician-assistants.htm Back to text ↑
- National Center for Health Workforce Analysis. Workforce Projections. Accessed April 1, 2024. https://data.hrsa.gov/topics/health-workforce/workforce-projections Back to text ↑
- Salsberg E, Quigley L. Are we facing a physician assistant surplus? JAAPA. 2016;29(11):40-44. doi:10.1097/01.JAA.0000502865.59093.ef Back to text ↑
- Salsberg E. Changes in the Pipeline of New NPs and RNs: Implications for Health Care Delivery and Educational Capacity. Health Affairs Blog. Published online 2018. doi:10.1377/hblog20180524.993081 Back to text ↑
- Auerbach DI, Buerhaus PI, Staiger DO. Implications of the rapid growth of the nurse practitioner workforce in the US. Health Aff (Millwood). 2020;39(2):273-279. doi:10.1377/hlthaff.2019.00686 Back to text ↑
- Salsberg E. Changes in the Pipeline of New NPs and RNs: Implications for Health Care Delivery and Educational Capacity. Health Affairs Blog. Published online 2018. doi:10.1377/hblog20180524.993081 Back to text ↑
- Volpe KD. NP and PA Presidents Discuss Workforce Shortage and the Future. Clinical Advisor. Published January 12, 2023. Accessed March 15, 2024. https://www.clinicaladvisor.com/home/topics/practice-management-information-center/nps-pas-best-health-care-jobs/ Back to text ↑
- Wallace C. Why NPs have the best job in healthcare. Published January 11, 2024. Accessed March 15, 2024. https://www.beckersasc.com/asc-news/why-nps-have-the-best-job-in-healthcare.html Back to text ↑
- Masson G. Unemployment rate, job outlook for 7 healthcare jobs. Published February 4, 2021. Accessed March 15, 2024. https://www.beckershospitalreview.com/hospital-management-administration/unemployment-rate-job-outlook-for-7-healthcare-jobs.html Back to text ↑
- U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. Technical Documentation for HRSA’s Health Workforce Simulation Model. Published September 2022. Accessed October 3, 2022. https://bhw.hrsa.gov/data-research/projecting-health-workforce-supply-demand/technical-documentation Back to text ↑
- Smith CD, Balatbat C, Corbridge S, et al. Implementing Optimal Team-Based Care to Reduce Clinician Burnout. NAM Perspectives. Published online September 17, 2018. doi:10.31478/201809c Back to text ↑
- American College of Obstetricians and Gynecologists. Collaboration in Practice: Implementing Team Based Care. 2016. https://www.acog.org/-/media/project/acog/acogorg/clinical/files/task-force-report/articles/2016/collaboration-in-practice-implementing-team-based-care.pdf Back to text ↑
- Fiscella K, McDaniel SH. The complexity, diversity, and science of primary care teams. Am Psychol. 2018;73(4):451-467. doi:10.1037/amp0000244 Back to text ↑
- Bazemore A, Wingrove P, Peterson L, Petterson S. The diversity of providers on the family medicine team. J Am Board Fam Med. 2016;29(1):8-9. doi:10.3122/jabfm.2016.01.150229 Back to text ↑
- Rodriguez HP, Giannitrapani KF, Stockdale S, Hamilton AB, Yano EM, Rubenstein LV. Teamlet structure and early experiences of medical home implementation for veterans. J Gen Intern Med. 2014;29 Suppl 2(Suppl 2):S623-631. doi:10.1007/s11606-013-2680-1 Back to text ↑
- Sinsky CA, Sinsky TA, Althaus D, Tranel J, Thiltgen M. Practice profile. “Core teams”: nurse-physician partnerships provide patient-centered care at an Iowa practice. Health Aff (Millwood). 2010;29(5):966-968. doi:10.1377/hlthaff.2010.0356 Back to text ↑
- Buerhaus PI, Skinner J, McMichael BJ, et al. The integrity of MACRA may be undermined by “incident to billing” coding. Health Affairs Forefront. doi:10.1377/forefront.20180103.135358 Back to text ↑
- Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System. 2019. https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/jun19_medpac_reporttocongress_sec.pdf Back to text ↑
- Patel SY, Huskamp HA, Frakt AB, et al. Frequency of indirect billing to medicare for nurse practitioner and physician assistant office visits. Health Aff (Millwood). 2022;41(6):805-813. doi:10.1377/hlthaff.2021.01968 Back to text ↑
- Everett C, Christy J, Batchelder H, et al. Impact of primary care usual provider type and provider interdependence on outcomes for patients with diabetes: a cohort study. BMJ Open Qual. 2023;12(2). doi:10.1136/bmjoq-2022-002229 Back to text ↑
- Everett CM, Christy J, Morgan PA, et al. When is caring sharing? Primary care provider interdependence and continuity of care. JAAPA. 2023;36(1):32-40. doi:10.1097/01.JAA.0000902896.51294.47 Back to text ↑
- Everett CM, Docherty SL, Matheson E, et al. Teaming up in primary care: membership boundaries, interdependence, and coordination. JAAPA. 2022;35(2):1-10. doi:10.1097/01.JAA.0000805840.00477.58 Back to text ↑
- Karan A, DeUgarte D, Barry M. Medical “brain drain” and health care worker shortages: how should international training programs respond? AMA J Ethics. 2016;18(7):665-675. doi:10.1001/journalofethics.2016.18.7.ecas1-1607 Back to text ↑
- Runnels V, Labonté R, Packer C. Reflections on the ethics of recruiting foreign-trained human resources for health. Hum Resour Health. 2011;9(1):2. doi:10.1186/1478-4491-9-2 Back to text ↑
- Fraher E, Brandt B. Toward a system where workforce planning and interprofessional practice and education are designed around patients and populations not professions. J Interprof Care. 2019;33(4):389-397. doi:10.1080/13561820.2018.1564252 Back to text ↑
- Frogner BK, Fraher EP, Spetz J, et al. Modernizing scope-of-practice regulations — time to prioritize patients. N Engl J Med. 2020;382(7):591-593. doi:10.1056/NEJMp1911077 Back to text ↑
- Frogner BK, Fraher EP, Spetz J, et al. Modernizing scope-of-practice regulations — time to prioritize patients. N Engl J Med. 2020;382(7):591-593. doi:10.1056/NEJMp1911077 Back to text ↑
- Weiner J. Expanding Scope of Practice After COVID-19. Penn LDI. Published February 12, 2021. https://ldi.upenn.edu/our-work/research-updates/expanding-scope-of-practice-after-covid-19/ Back to text ↑
- Langelier M, Surdu S, Goodwin N. Case Studies of 6 Safety Net Organizations That Integrate Oral and Mental/Behavioral Health With Primary Care Services. Center for Health Workforce Studies. Published February 22, 2019. https://www.chwsny.org/our-work/reports-briefs/case-studies-of-6-safety-net-organizations-that-integrate-oral-and-mentalbehavioral-health-with-primary-care-services/ Back to text ↑
- Sanchez K, Chapa T, Ybarra R, Jr ONM. Eliminating health disparities through culturally and linguistically centered integrated health care: consensus statements, recommendations, and key strategies from the field. J Health Care Poor Underserved. 2014;25(2):469-477. doi:10.1353/hpu.2014.0100
Back to text ↑ - Barraclough F, Smith-Merry J, Stein V, Pit S. Workforce development in integrated care: a scoping review. Int J Integr Care. 2021;21(4):23. doi:10.5334/ijic.6004
Back to text ↑ - Levengood TW, Peng Y, Xiong KZ, et al. Team-based care to improve diabetes management: a community guide meta-analysis. Am J Prev Med. 2019;57(1):e17-e26. doi:10.1016/j.amepre.2019.02.005
Back to text ↑ - Wagner EH, Flinter M, Hsu C, et al. Effective team-based primary care: observations from innovative practices. BMC Fam Pract. 2017;18(1):13. doi:10.1186/s12875-017-0590-8
Back to text ↑ - ACT Center. Primary Care Team Guide | ACT Center. Primary Care Team Guide | ACT Center. https://www.act-center.org/our-work/primary-care-transformation/team-based-care/learning-effective-ambulatory-practices Back to text ↑
- Chaney A, Beliles G, Keimig A, Porter I. Advanced practice provider care team models: best practices from an academic medical center. J Ambul Care Manage. 2022;45(2). https://journals.lww.com/ambulatorycaremanagement/Fulltext/2022/04000/Advanced_Practice_Provider_Care_Team_Models__Best.6.aspx
Back to text ↑ - Nelson S, Turnbull J, Bainbridge L, et al. Optimizing Scopes of Practice: New Models of Care for a New Health Care System. 2014. https://cahs-acss.ca/wp-content/uploads/2015/07/Optimizing-Scopes-of-Practice_REPORT-English.pdf Back to text ↑
- Leslie K, Moore J, Robertson C, et al. Regulating health professional scopes of practice: comparing institutional arrangements and approaches in the US, Canada, Australia and the UK. Hum Resour Health. 2021;19(1):15. doi:10.1186/s12960-020-00550-3 Back to text ↑
- Frogner BK, Fraher EP, Spetz J, et al. Modernizing scope-of-practice regulations — time to prioritize patients. N Engl J Med. 2020;382(7):591-593. doi:10.1056/NEJMp1911077 Back to text ↑
- Buerhaus PI, Skinner J, McMichael BJ, et al. The integrity of MACRA may be undermined by “incident to billing” coding. Health Affairs Forefront. doi:10.1377/forefront.20180103.135358
Back to text ↑ - Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System. 2019. https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/jun19_medpac_reporttocongress_sec.pdf Back to text ↑
- Patel SY, Huskamp HA, Frakt AB, et al. Frequency of indirect billing to Medicare for nurse practitioner and physician assistant office visits. Health Aff (Millwood). 2022;41(6):805-813. doi:10.1377/hlthaff.2021.01968
Back to text ↑ - Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759
Back to text ↑ - Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. doi:10.1370/afm.1713
Back to text ↑ - Nundy S, Cooper LA, Mate KS. The quintuple aim for health care improvement: a new imperative to advance health equity. JAMA. 2022;327(6):521-522. doi:10.1001/jama.2021.25181
Back to text ↑

