Executive Summary
Successful health policy focuses, in part, on timely access to care, which requires an adequate health workforce to meet the needs of the population. In the United States, federal and state health policymakers provide funding for health professions education and training, research to assess and inform the adequacy of the health workforce, efforts to distribute the workforce where geographic or specialty gaps are identified, and the development of tools to project the size, composition, and need for the health workforce in the future.
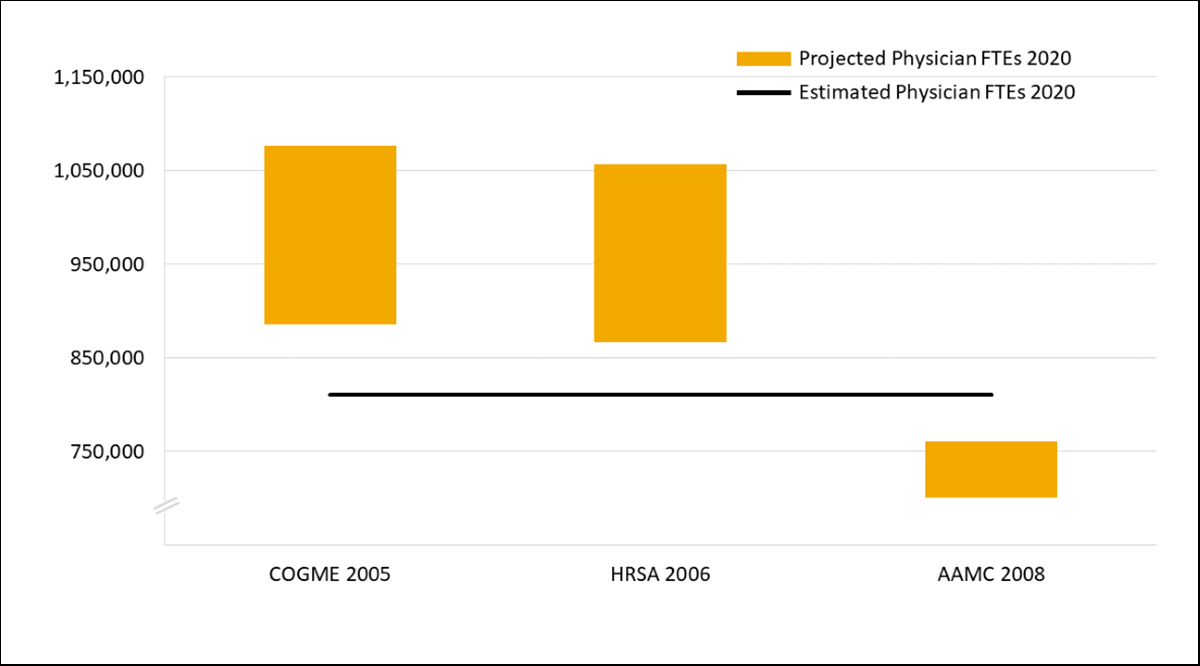
One of those tools is workforce projections modeling, which, over the past decade, has consistently projected vast future shortages of health care workers, especially physicians. Previous long-term national workforce projections of the future supply of physicians over the past two decades have not been precisely accurate (Figure 1) and have focused exclusively on shortages of primary care professionals despite increasing evidence that shortages in physician subspecialties and many other types of health care workers are more severe.
While not disregarding these projections entirely, policymakers have nonetheless not found them compelling — and have relied on technology, major shifts in the roles of health care professionals, and dramatic changes in patient behavior to solve the shortage problem.
This paper from the AAMC Research and Action Institute examines the history of health workforce projections modeling in the United States, with a goal of assessing the validity of various approaches. While workforce projections modeling efforts can be accurate and have been effective in alerting policymakers and other stakeholders to possible future shortages of specific health professions and occupations, they suffer from several important deficits: (1) lack of data, (2) being stuck in workforce silos, and (3) inadequate distribution and location modeling. The paper will inform policymakers and researchers of these limitations and future work needed to improve the projections, including the need to move away from physician-focused modeling to more services-based models that integrate the contributions of health care workers beyond physicians.
Introduction
The COVID-19 pandemic has disrupted life in the United States, upending social, economic, and political institutions. At the outset of the pandemic, there was a tremendous need for health workers to act as the surge workforce for hospitals and intensive care units in urban hotspots across the country. The experience in New York provides an example of what was happening at the time. In late March 2020, New York called for volunteers across the state and the nation to help create a surge health workforce in response to the burgeoning pandemic.1 More than 90,000 people responded.2 Hospitals developed new recruiting processes on the fly, relying heavily on contracts with travel nurse agencies to staff their facilities.2,3
The experience of NYC Health + Hospitals — New York City’s public health care system — illustrates the mammoth lengths to which some hospitals had to go to build and deploy surge workforces during the pandemic. They redeployed existing staff from non-intensive care to intensive care duties; recruited additional staff from among volunteers and contractors from recruiting and travel nurse agencies; designed new, streamlined onboarding and training processes from scratch; used technology to facilitate the coordination of their efforts; and employed rapid-cycle quality improvement techniques to evaluate and hone these new operations.3,4
Why did these hospitals find themselves needing to go to such lengths, cobbling together new and complex staffing systems on the fly? They were already experiencing workforce challenges and did not have adequate tools to help them adapt to the sudden onset of a public health emergency. Successful health policy focuses, in part, on timely access to care, which requires an adequate health workforce to meet the needs of the population. Federal health policy addresses the problem by providing funding for health professions education and training, research to assess and inform the adequacy of the health workforce, efforts to distribute the workforce where geographic or specialty gaps are identified, and the development of tools to project the size, composition, and need for the health workforce in the future.5
This paper explores some of those tools with a focus on workforce projections models. With an eye to making them more useful for health policy decisions to ensure an adequate workforce in the future, the paper identifies several important deficits of common projections models: (1) lack of data, (2) being stuck in workforce silos, and (3) inadequate distribution and location modeling.
In Addition to Being Better Prepared for Future Pandemics and Public Health Emergencies, Why Do We Need to Model Future Health Workforce Adequacy?
In addition to being better prepared, being able to anticipate the size, composition, and other characteristics of the health workforce required to meet the needs of the population is important to health policy for several reasons.
- Expanding existing or building new training infrastructure takes substantial time, planning effort, and financing. For example, it can take five to 10 years for a new medical school to be developed and built and cost hundreds of millions of dollars in capital expenditures and personnel before new medical students begin to graduate from the institution.
- While the process varies for different professions, it can take many years to produce a new member of the health workforce. The training requirements for physicians, for example, include four years of undergraduate education, three or four years of medical school, and anywhere from three to seven years of residency and/or fellowship training. Registered nurses require two to four years of training, and advanced practice nurses, an additional two to four years before they can practice.6
- The health workforce is not a static body. New people join the workforce as they complete their training and meet the requirements to practice in a health profession. Members of the workforce provide care and services at various levels of effort in health care settings. The correlates of this variation include age, practice or work location, and occupation, profession, or specialty. Finally, as with many other professions, members of the workforce leave it, as well.
Due to the length of time and money required to start new health professions training efforts and to the ever-changing workforce, knowing how many health professionals there will be in the future and whether the workforce will be adequate to meet the needs of the population, including during public health emergencies, is vital. Workforce projections models are intended to help policymakers, the health professions education community, and those providing care plan for and direct resources effectively.
The Language of Health Workforce Projections Modeling
The terminology around workforce projections models is important to understand. Three terms often used in workforce projections are supply, demand, and need.
Supply, demand, and need
Supply generally refers to those providing health care to the population. Some projections will take into account classifications within specific professions and occupations. For example, the physician supply is often classified by individual medical specialty or broader groups of specialties (primary care, surgery, medicine specialties). Supply is often expressed as the health care services that can be provided by a population of health care providers.7
Demand is an economic concept based on patients’ or payers’ willingness to purchase health care services at a particular price. In projections modeling, it generally refers to the amount of health workforce required to provide the volume of health care services the population wants to obtain through the market at a point in time. Demand depends on social and cultural factors associated with health literacy, access to services, willingness to seek services, insurance status, price, geography, and availability of services.7-9 Like supply, it can be defined in terms of the health workforce itself or a volume of health care services.
Need refers to the amount of health workforce required to provide a volume of services necessary to achieve a desired health standard. It is a normative, subjective assessment of the ideal health workforce required to provide health services in an area or to a population to maintain their health regardless of ability to pay or what level of services are actually available at a point in time. As such, need is generally closely tied to the disease burden in a particular place or population.7-12 Like demand and supply, it can be defined in terms of the health workforce itself or a volume of health care services.
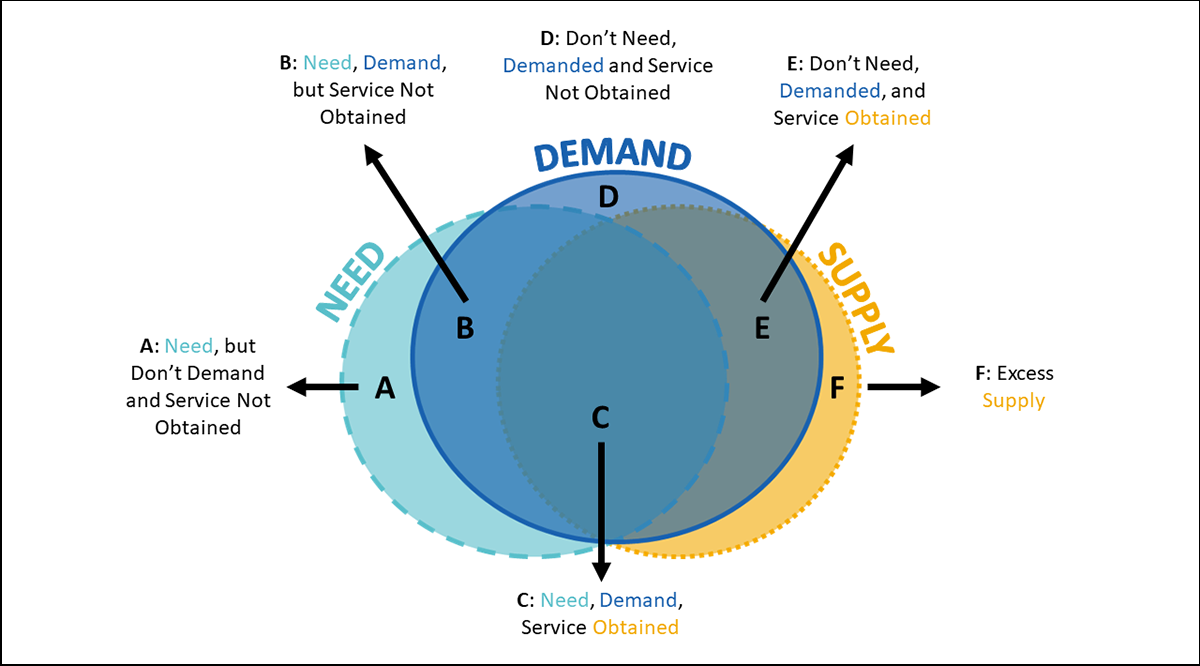
The intersection of supply, demand, and need: What’s a shortage?
To determine whether workforce supply is adequate, supply, demand, and/or need are compared. Given the definitions of supply, demand, and need above, understanding how those can intersect helps refine the concept of a workforce shortage.
Ideally, supply, demand, and need would coincide as illustrated in the area labeled C in Figure 1. However, when stakeholders identify shortages in the health workforce, they are describing situations where individuals cannot obtain the services they demand due to not being able to access those services, perhaps related to inadequate insurance coverage13 or scarcity of providers14 (Areas B and D), or to need due to not seeking medical care at all, perhaps related to low health literacy15 (Area A). Further, there can be situations where services are demanded and received but not needed (Area E), such as supply-induced demand and those where there are excess providers (Area F), meaning beyond what is needed or demanded.16,17 The intersection of supply, demand, and need can be experienced differently by population groups defined by characteristics such as race, ethnicity, insurance status, economic status, and geographic location. Health policy aims to expand Area C while minimizing Areas A, B, D, E, and F.
Singular focus on individual professions and occupations
Almost all projections modeling focuses on one profession or occupation. Physician workforce projections models, made at various times over the past century, are the most well-known examples of health workforce modeling.18 The Graduate Medical Education National Advisory Committee’s (GMENAC’s) work in the late 1970s and early 1980s was one of the first national-level in-depth efforts to project the supply and need for physicians.19 Although single profession and occupation projections remain common, there have been exceptions to a singular focus that have continued the movement toward broader workforce models.20 For example, the Primary Care Integrated Requirements Model by the Health Resources and Services Administration (HRSA), developed in the 1990s, sought to project the required supply of primary care practitioners, including primary care physicians, nurse practitioners, physician assistants, and certified nurse midwives,21 and more recently, HRSA introduced a model that includes more than 30 health professions.20
Projections and predictions
Understanding the distinction between projections and predictions is vital. Predictions are statements that refer to what will happen in the future.9,22 They can be made when one has a high degree of certainty about how today’s conditions are going to change or a high degree of certainty that they are not going to change in the future. Accurate predictions can generally not be made about health workforce supply, demand, or need because they are influenced by a multitude of factors, including the political proclivities of policymakers, technological advancements, and economic trends, as well as a multitude of individual decisions made and actions taken by health care providers and the populations they serve on a daily basis. Projections, on the other hand, describe what may happen in the future, given certain well-defined assumptions about current and future conditions and, in some cases, the changing structure of a system over time. Projections and predictions may also change the behavior of clinicians (e.g., students who might avoid a specialty or profession projected to be surplus in the future) or of policymakers (e.g., altering funding for training or clinical care for professions projected to be in shortage in the future). For policymakers, the value of projections thus lies in their ability to demonstrate the implications of current and emerging trends to which policymakers can respond.23
Common Health Workforce Projections Models24
Stock and flow
Stock-and-flow models depict the health workforce and incorporate change over time in a format that is relatively easy to understand. These models treat workforce and population cohorts as stocks of resources, and movements between those stocks as flows of resources. In health workforce modeling, they start with the current health workforce supply and demand or need, typically delineated by age cohort (the stocks). On the supply side, the models then project forward in time using parameters that estimate incoming members of the workforce based on the number of people who complete training each year, those who return to the workforce after having temporarily left, and entrants from other countries. That number is then reduced by the estimates of those who retire, become inactive, or die. On the demand-need side, the models project forward in time using parameters that estimate the demand or need, such as historical utilization rates or rate targets based on a desired level of service. The process is repeated for future years until the target year is reached.7,15
Microsimulation
The microsimulation modeling approach, a relatively novel one, moves away from the idea of stocks and flows and builds on the individual as the unit of analysis. The health care seeking (demand) and labor market participation (supply) behaviors of the individual become the building blocks for calculating estimates for populations of interest. For example, in a recent demand microsimulation model based on an individual’s characteristics, use of health care services was simulated using parameters derived from equations relating those characteristics to health care utilization. Then, the number and mix of health care providers required to meet the demand for services were estimated using parameters derived from patterns of provider productivity in different settings.25-28 In terms of workforce supply, the microsimulation approach bases projections on how provider characteristics — typically age, gender, occupation, specialty, setting — relate to labor market participation behaviors, including actively working, hours spent in practice, and retirement. Parameters derived from equations describing those relationships are applied to a population of providers to generate projections of the supply at a point in time.27,29
System dynamics
A system dynamics approach begins with the recognition that human behavior is uncertain and nonlinear and occurs within complex, dynamic systems. System dynamics is rooted in the theory of nonlinear dynamics and feedback control developed in the fields of mathematics, physics, and engineering and applied to human behavior and interaction and the systems that build up around behavior and interactions over time. System dynamics models are typically built from stock-and-flow structures where flows between stocks are based causally on other values of factors within the system and on an endogenous understanding of the structures generating these trends over time, time delays, and reinforcing and balancing feedback loops.30
Examples of system dynamics modeling in the U.S. health workforce domain include dynamic simulation models of the local physician workforce in Cleveland, Ohio, and Albuquerque, New Mexico31; the dynamics of workplace stress among nursing aides32; demand for ambulatory care services33; and work commissioned by the American Association of Physicists in Medicine to project the supply and demand for medical physicists using a dynamic stock-and-flow model focused on a changing training and certification process.34 Additional examples of system dynamics modeling in the health workforce can be found in the international peer-reviewed literature.35
Historical Projections Modeling
While it might not be possible to predict when the next pandemic or public health emergency will occur, is it possible to project future health workforce supply using the kinds of models described above? To shed some light on that question, we compiled several historical national projections of physician full-time-equivalent (FTE) supply for 2020 made between 2005 and 2019 by different modeling teams using different methods (Figure 2). These projections were selected because they are publicly available, are at the same geographic level, and represent several of the approaches described above. The purpose of the comparison is not to suggest one is better than another, nor is it to systematically assess each model’s assumptions and limitations. Rather, it is to get a measure of how accurate projections have been historically. For each, we recorded the minimum and maximum projection for the FTE physician supply in 2020. Given what we stated about projections, the reader should expect that the projections will not predict the actual estimates of physicians in 2020. We might, however, expect that projections made closer to 2020 would likely be closer to actual FTE counts because there would have been less opportunity for the conditions underlying the projections to change.
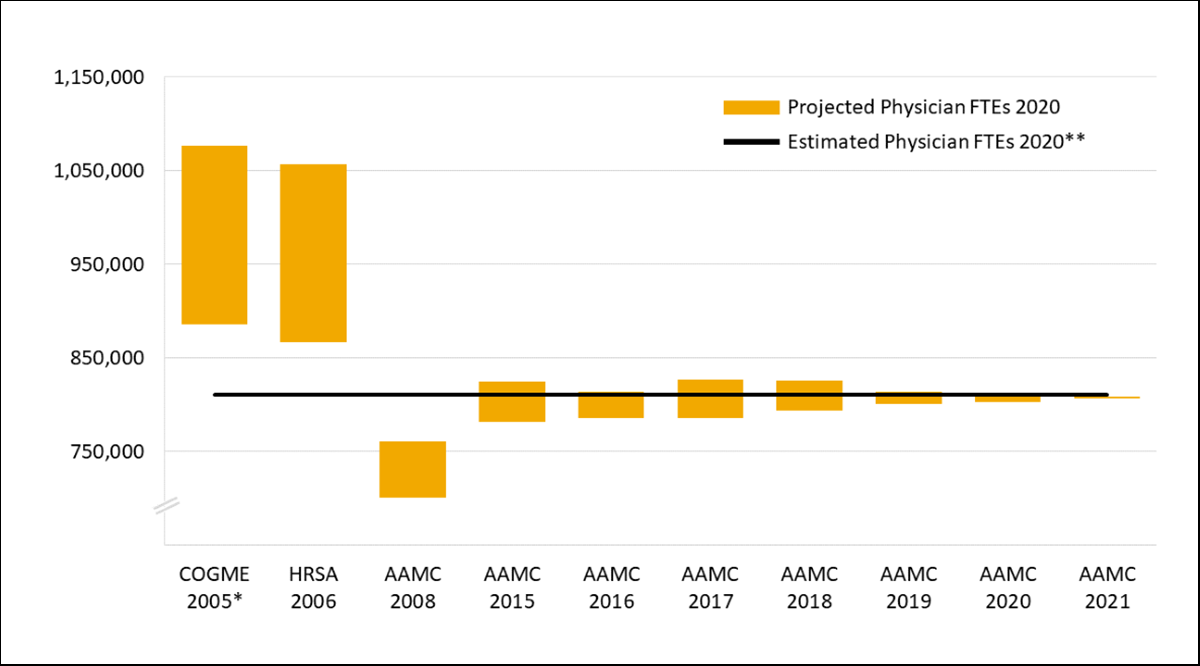
In half the historical projections of physician supply we reviewed, the estimated number of physician FTEs in 2020 fell within the projected range. The earlier projection efforts were further away from the 2020 estimate, with some projection ranges greater than the estimate and one projection range less than the estimate. The results of these comparisons were not unexpected. Salsberg and Forte36 found similar outcomes when reviewing physician workforce trends from 1980 to 2020 following the GMENAC physician workforce projections from the late 1970s.
Important Workforce Projections Modeling Deficits
While workforce projections modeling efforts can be accurate and have been effective in alerting policymakers and other stakeholders to possible future shortages of certain, specific health professions and occupations, they do suffer from several important deficits: (1) lack of data, (2) being stuck in workforce silos, and (3) inadequate distribution and location modeling.
Lack of robust data for improved modeling
One commonality running through all workforce projections modeling efforts is a reliance on robust, timely, and accurate data. Without those, projections cannot be made effectively or with any confidence. Moreover, the more advanced modeling techniques, such as microsimulation and system dynamics, require a quality and quantity of data that are often unavailable. As Buntin and colleagues37 recently pointed out, the models the AAMC and HRSA have been developing have intense data requirements. Data on the numbers of newly trained physicians and other members of the health workforce, hours worked, retirement patterns, population characteristics, current care delivery patterns and utilization, and the availability of other potential health care providers are not always available, timely, or representative of the experiences of the diversity among population groups. The continued development of better, more refined projections models is challenged by an inadequate investment in data and the underlying research that analysis of those data would provide.
Stuck in workforce silos
Earlier in this paper, we stated that most projections modeling efforts focus on a specific profession or occupation. That is, a profession is considered in and of itself in a vacuum, effectively siloed from other professions and occupations that it interacts with in providing care for patients. In reality, health care is provided in an interconnected way, with many professions and occupations playing roles and working together in the delivery of care to the population. Health workforce projections models should reflect this reality if they are going to continue to be helpful in informing health workforce policy decisions going forward.
This modeling deficit is the result of several factors, including variable regulation of health professions by state,38-40 overlapping scopes of practice and skills,41 barriers and facilitators of interprofessional practice, and a lack of research on the variation in how care is provided, including who contributes to care, what each participant contributes, and whether those contributions vary across kinds of care (e.g., primary, specialty-specific, behavioral health), characteristics of patients (e.g., insurance type, age, race/ethnicity), and geography (e.g., across the urban-rural continuum, state to state).
Research is needed to uncover and understand the dynamics of interprofessional practice and new integrated models of care. We need to explore, for example, how the relationship between supply and demand or need affects care delivery within and between professions and occupations; how workforce outcomes like labor force participation, job satisfaction, and clinician wellness affect and are affected by those dynamics, interprofessional practice, and new integrated models of care; and how these workforce aspects affect interest in particular professions and occupations.
Distribution and location: Place matters
Another deficit many projections modeling efforts suffer from is not being able to project how practitioners distribute and make practice-location decisions. In addition to concerns about overall shortages among the health workforce, it has long been observed that shortages are more severe in some places than in others. One illustration of maldistribution in the health workforce is the uneven distribution of physicians across the rural-urban continuum. For example, rural areas have historically and continue to experience severe shortages of health care resources.42,43 Workforce shortages and other access challenges are experienced in all types of areas, but too often, projections models fail to adequately account for location. In some previous projection efforts — for example, the 2005 COGME44 physician supply projections and the GMENAC projections in the late 1970s — subnational practice-location projections (i.e., at local, state, and regional levels) were not modeled at all. In some state physician supply projections modeling efforts, such as in Michigan45 and New York,46 practice-location decisions were modeled as a function of demand growth. More recently, modelers have relied on patterns of migration from state to state.19
Despite literature that identifies factors influencing physician migration decisions and patterns, little work has been done to incorporate more than the migration functions listed above into projections models. Insights like those from Holmes and Fraher,47 Chou and Lo Sasso,48 and, most recently, Hu and colleagues49 on practice-location decisions would greatly enhance the current physician supply projections models. Expanding research efforts like these to other professions, occupations, and models of care could further enhance existing projections models.
Preparing for the Next Pandemic
At the outset of this paper, we described some of the results of being ill-prepared for the COVID-19 pandemic. Since 2020, the health workforce has been pushed to its limits and beyond. Preparing for the future and the next pandemic or public health emergency will require making informed health policy decisions around allocating and targeting resources for the education and training of the health workforce.50 Those decisions will require information about (1) what future workforce requirements may be, including where and what kinds of services may be sought, and (2) what workforce supply may be available, including the composition and location of the workforce. Health workforce projections models are one of the most important tools for guiding these decisions. Armed with information from those models, health policy discussions and decisions about how to better ensure health workforce adequacy in the future can occur — so that we are better prepared for the next public health emergency.
Final Thoughts
Health workforce projections are often criticized because they become associated with the policy recommendations they inform. Advocates of particular policy options criticize projections models that do not support their favored policy options. For example, part of the critical response to the 16th report from COGME’s recommendations to increase physician education and training to combat a projected shortage of physicians in 202040 was that the projections did not fully account for the growing contributions of other professionals in the delivery of care to the population and questions around whether adding more physicians would make a more effective health care system.51,52 Those were valid criticisms — the models informing COGME’s recommendations were not capable of addressing those questions. It is important to recognize that criticisms like these do not call into question the value of workforce projections modeling, rather, they highlight their limitations and the need to understand their underlying assumptions. These and similar criticisms have laid the groundwork for improving the models and the useful information they produce to address important policy questions. But more improvements are needed, and other questions require answers.
In the past decade and a half, health workforce policy priorities related to the adequacy of the workforce to meet the requirements of the population have become more refined. First, with the passage of the Affordable Care Act in 2010, the goals of the Triple Aim for the health care system — improving population health, enhancing the care experience, and reducing costs53 — became evident. Those were followed shortly by the addition of a fourth aim — clinician wellness.54 Most recently, a fifth aim — health equity and the importance of diversity55 — has been elevated as an explicit priority for health care system improvement. Given these system goals and potentially greater demands on clinicians, the workforce projections models that inform policy decisions about the future should have the capacity to address the health workforce policy priorities related to workforce supply, demand, and need. The projections model improvements outlined above offer several steps for moving the models in that direction.
Notes
- Feuer W, Mangan D, Lovelace Jr B. New York Gov. Cuomo issues nationwide call for doctors and nurses as state battles worst coronavirus outbreak in US. CNBC. March 30, 2020. https://www.cnbc.com/2020/03/30/coronavirus-fight-new-york-gov-cuomo-issues-nationwide-call-for-doctors-and-nurses.html. Accessed Nov. 6, 2022.
- Beasley D, Cooke, K. New York City hospitals cancel temporary workers as coronavirus cases stabilize. Reuters. April 15, 2020. https://www.reuters.com/article/us-health-coronavirus-newyork-staffing-idUSKCN21X00X. Accessed Nov. 6, 2022.
- Keeley C, Jimenez J, Jackson H, et al. Staffing up for the surge: expanding the New York City public hospital workforce during the COVID-19 pandemic. Health Aff. 2020;39(8):1426-1430. doi:10.1377/hlthaff.2020.00904.
- Uppal A, Silvestri DM, Siegler M, et al. Critical care and emergency department response at the epicenter of the COVID-19 pandemic. Health Aff. 2020;39(8):1443-1449. doi:10.1377/hlthaff.2020.00901.
- Ricketts TC. Building an effective and sustainable health care workforce (1960s-present). In: Oliver TR, ed. Guide to U.S. Health and Health Care Policy. 1st ed. Washington, DC: CQ Press; 2014;197-212.
- U.S. Bureau of Labor Statistics. Occupational Outlook Handbook: Registered Nurses. https://www.bls.gov/ooh/healthcare/registered-nurses.htm#tab-4. Last modified Sept. 8, 2022. Accessed Oct. 10, 2022.
- Safarishahrbijari A. Workforce forecasting models: a systematic review. J Forecast. 2018;37(7):739-753. doi:10.1002/for.2541.
- Wing P, Armstrong D, Forte G, Moore J. Health Workforce Analysis Guide. Rensselaer, NY: Health Workforce Technical Assistance Center; 2016. https://www.healthworkforceta.org/wp-content/uploads/2016/11/Health-Workforce-Analysis-Guide_2016-E…. Published October 2016. Accessed Oct. 12, 2022.
- Dill MJ, Salsberg ES. The Complexities of Physician Supply and Demand: Projections Through 2025. Washington, DC: Center for Workforce Studies, AAMC; 2008. bit.ly/3qmwaLT.
- Fries JF, Koop CE, Sokolov J, Beadle CE, Wright D. Beyond health promotion: reducing need and demand for medical care. Health Aff. 1998;17(2):70-84. doi:10.1377/hlthaff.17.2.70.
- Turner LA, Østbye T, Pederson LL. Work force planning in the 90s, part I: efficiency, economy and political will — the need for a new approach. Healthc Manage Forum. 1993;6(1):34-40. doi:10.1016/S0840-4704(10)61119-2.
- Jacoby I. Forecasting requirements for physical therapists. Phys Ther. 1995;75(1):38-44. doi:10.1093/ptj/75.1.38.
- Seo V, Baggett TP, Thorndike AN, et al. Access to care among Medicaid and uninsured patients in community health centers after the Affordable Care Act. BMC Health Serv Res. 2019;19(1):291. doi:10.1186/s12913-019-4124-z.
- Liu J. Health professional shortage and health status and health care access. J Health Care Poor Underserved. 2007;18(3):590-598. doi:10.1353/hpu.2007.0062.
- Morris NS, Field TS, Wagner JL, et al. The association between health literacy and cancer-related attitudes, behaviors, and knowledge. J Health Commun. 2013;18(Suppl 1):223-241. doi:10.1080/10810730.2013.825667.
- Folland S, Goodman AC, Stano M. The Economics of Health and Health Care. 7th ed. Milton Park, UK: Routledge; 2016. doi:10.4324/9781315510736.
- Wennberg J. Wrestling with variation: an interview with Jack Wennberg [interviewed by Fitzhugh Mullan]. Health Aff (Project Hope). 2004;23(Suppl 2):VAR-73-VAR-80. doi:10.1377/hlthaff.var.73.
- Ricketts TC. The health care workforce: will it be ready as the boomers age? A review of how we can know (or not know) the answer. Annu Rev Public Health. 2011;32(1): 417-430. doi:10.1146/annurev-publhealth-031210-101227.
- Graduate Medical Education National Advisory Committee. Report of the Graduate Medical Education National Advisory Committee to the Secretary, Department of Health and Human Services—Volume II: Modeling, Research, and Data Technical Panel (HRA 81-652). Washington, DC: U.S. Department of Health and Human Services, Public Health Service, Health Resources Administration; 1981.
- Council on Graduate Medical Education and National Advisory Council on Nurse Education and Practice. Report on Primary Care Workforce Projections. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, Health Resources Administration; 1995.
- National Center for Health Workforce Analysis. Technical Documentation for HRSA’s Health Workforce Simulation Model. Washington, DC: U.S. Department of Health and Human Services, Health Resources and Services Administration; 2022. https://bhw.hrsa.gov/data-research/projecting-health-workforce-supply-demand/technical-documentation. Date last reviewed: December 2022.
- MacCracken M. Prediction versus projection—forecast versus possibility. Guest editorial. WeatherZine. https://sciencepolicy.colorado.edu/zine/archives/1-29/26/guest.html. Published February 2001. Accessed Oct. 4, 2022.
- Roberfroid D, Leonard C, Stordeur S. Physician supply forecast: better than peering in a crystal ball? Human Resour Health. 2009;7(1):1-13. doi.org/10.1186/1478-4491-7-10.
- Other projections modeling approaches are used to a lesser extent in the health workforce domain (e.g., Markov chain models, optimization models, and regression models). Interested readers might consider reviewing sources in notes 7 and 23.
- Dall TM, Chakrabarti R, Storm MV, Elwell EC, Rayburn WF. Estimated demand for women’s health services by 2020. J Womens Health (Larchmt). 2013 Jul;22(7):643-648. doi:10.1089/jwh.2012.4119.
- Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff. (Millwood). 2013;32(11):2013-2020. doi:10.1377/hlthaff.2013.0714.
- Dall TM, Storm MV, Chakrabarti R, et al. Supply and demand analysis of the current and future US neurology workforce. Neurology. 2013;81(5):470-478. doi:10.1212/WNL.0b013e318294b1cf.
- AAMC. The Complexities of Physician Supply and Demand: Projections from 2013-2025. Washington, DC: Association of American Medical Colleges; 2015.
- National Center for Health Workforce Analysis. Modeling Supply of Health Professionals: II. Supply Modeling Overview. Washington, DC: U.S. Department of Health and Human Services, Health Resources and Services Administration; 2022. https://bhw.hrsa.gov/data-research/projecting-health-workforce-supply-demand/technical-documentatio…. Accessed Oct. 3, 2022.
- Richardson GP. Reflections on the foundations of system dynamics. Syst Dyn Rev. 2011;27(3):219-243. doi:10.1002/sdr.462.
- Dill MJ, Hirsch GB. The Association of American Medical Colleges’ Local area physician workforce modeling project. Acad Med. 2021;96(10):1393-1400. doi:10.1097/ACM.0000000000004133.
- Jetha A, Kernan L, Kurowski A, Pro-Care Research Team. Conceptualizing the dynamics of workplace stress: a systems-based study of nursing aides. BMC Health Serv Res. 2017;17:12. doi:10.1186/s12913-016-1955-8.
- Diaz R, Behr J, Tulpule M. A systems dynamics model for simulating ambulatory health care demands. Simul Healthc. 2012;7(4):243-250. doi:10.1097/SIH.0b013e318259d134.
- Forte G. Modeling Medical Physicist Supply and Demand. Talk presented at: AAPM 52nd Annual Meeting; July 21, 2010; Philadelphia, PA. https://www.aapm.org/meetings/amos2/pdf/49-14390-28043-305.pdf. Accessed Oct. 14, 2022.
- Darabi N, Hosseinichimeh N. System dynamics modeling in health and medicine: a systematic literature review. Syst Dyn Rev. 2020;36(1):29-73. doi:10.1002/sdr.1646.
- Salsberg ES, Forte GJ. Trends in the physician workforce, 1980-2000. Health Aff (Millwood). 2002;21(5):165-173. doi:10.1377/hlthaff.21.5.165.
- Buntin MB, Connell J, Buerhaus P. Projecting the health care workforce needed in the US. JAMA Health Forum. 2022;3(8):e222430-e222430. doi:10.1001/jamahealthforum.2022.2430.
- Langelier M. Innovations in scope of practice. Guest editorial. Dimens Dent Hyg. 2020;18(1):16-17.
- Langelier M, Continelli T, Moore J, Baker B, Surdu S. Expanded scopes of practice for dental hygienists associated with improved oral health outcomes for adults. Health Aff (Millwood). 2016;35(12):2207-2215. doi:10.1377/hlthaff.2016.0807.
- Moore J, Goodwin N. Expanding access to care with scope of practice. Dimens Dent Hyg. 2019;17(3):12-14.
- Holmes GM, Morrison M, Pathman DE, Fraher E. The contribution of “plasticity” to modeling how a community’s need for health care services can be met by different configurations of physicians. Acad Med. 2013;88(12):1877-1882. doi:10.1097/ACM.0000000000000026.
- Ricketts TC. The changing nature of rural health care. Annu Rev Public Health. 2000;21(1):639-657. doi:10.1146/annurev.publhealth.21.1.639.
- Council on Graduate Medical Education. Strengthening the Rural Health Workforce to Improve Health Outcomes in Rural Communities: 24th Report. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, Health Resources Administration; 2022. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/graduate-medical-edu/reports/cogm…. Published April 2022. Accessed Oct. 16, 2022.
- Council on Graduate Medical Education. Physician Workforce Policy Guidelines for the United States, 2000-2020: Sixteenth Report. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, Health Resources Administration; 2005. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/graduate-medical-edu/reports/jan-…. Published January 2005. Accessed Oct. 16, 2022.
- Forte G, Armstrong D. Michigan Supply and Demand Through 2020. Albany, NY: University at Albany, State University of New York, Center for Health Workforce Studies; 2007. https://www.chwsny.org/wp-content/uploads/2015/09/miforecast2007.pdf. Published January 2007. Accessed Oct. 16, 2022.
- Forte G, Moore J, Armstrong D, McGinnis S, Dionne M. New York Physician Supply and Demand through 2030. Albany, NY: University at Albany, State University of New York, Center for Health Workforce Studies; 2010. https://www.chwsny.org/our-work/reports-briefs/r-2010-7. Published April 24, 2010. Accessed Oct. 16, 2022.
- Holmes GM, Fraher EP. Developing physician migration estimates for workforce models. Health Serv Res. 2017;52(1):529-545. doi:10.1111/1475-6773.12656.
- Chou CF, Lo Sasso AT. Practice location choice by new physicians: the importance of malpractice premiums, damage caps, and health professional shortage area designation. Health Serv Res. 2009;44(4):1271-1289. doi:10.1111/j.1475-6773.2009.00976.x.
- Hu X, Dill MJ, Conrad SS. What moves physicians to work in rural areas? An in-depth examination of physician practice location decisions. Econ Dev Q. 2022;36(3):245-260. doi:10.1177/08912424211046600.
- Grover A, Rasouli T, Pincus L, Lin A. The Way Forward Starts Now: Lessons From COVID-19. Washington, DC: AAMC; 2021. doi:10.15766/rai_bfr4tvxn.
- Goodman DC, Grumbach K. Does having more physicians lead to better health system performance? JAMA. 2008;299(3):335-337. doi:10.1001/jama.299.3.335.
- Phillips RL, Dodoo M, Jaen CR, Green LA. COGME’s 16th report to Congress: too many physicians could be worse than wasted. Ann Fam Med. 2005;3(3):268-270. doi:10.1370/afm.331.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759-769. doi:10.1377/hlthaff.27.3.759.
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. doi:10.1370/afm.1713.
- Nundy S, Cooper LA, Mate KS. The quintuple aim for health care improvement: a new imperative to advance health equity. JAMA. 2022;327(6):521-522. doi:10.1001/jama.2021.25181.
Figure 2 Sources
Council on Graduate Medical Education (COGME). Physician Workforce Policy Guidelines for the United States, 2000-2020: Sixteenth Report. Washington, DC: U.S. Department of Health and Human Services, Public Health Service, Health Resources and Services Administration (HRSA); 2005. U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions. Physician Supply and Demand: Projections to 2020. Washington, DC: Health Resources and Services Administration; 2006. Dill MJ, Salsberg ES. The Complexities of Physician Supply and Demand: Projections Through 2025. Washington, DC: Center for Workforce Studies, AAMC; 2008. Dall T, West T, Chakrabarti R, Iacobucci W. The Complexities of Physician Supply and Demand: Projections From 2014 to 2025. Washington, DC: Center for Workforce Studies, AAMC, and IHS Inc.; 2015. Dall T, West T, Chakrabarti R, Iacobucci W. The Complexities of Physician Supply and Demand: Projections From 2014 to 2025. Washington, DC: AAMC and IHS Markit; 2016. Dall T, Chakrabarti R, Iacobucci W, Hansari A, West T. The Complexities of Physician Supply and Demand: Projections From 2015 to 2030. Washington, DC: AAMC and IHS Markit Ltd.; 2017. Dall T, West T, Chakrabarti R, Reynolds R, Iacobucci W. The Complexities of Physician Supply and Demand: Projections From 2016 to 2030. Washington, DC: Center for Workforce Studies, AAMC, and IHS Markit Ltd; 2018. Dall T, Reynolds R, Jones K, Chakrabarti R, Iacobucci W. The Complexities of Physician Supply and Demand: Projections from 2017 to 2032. Washington, DC: Center for Workforce Studies, AAMC, and IHS Markit Ltd; 2019. Dall T, Reynolds R, Chakrabarti R, Jones K, Iacobucci W. The Complexities of Physician Supply and Demand: Projections from 2018 to 2033. Washington, DC: Center for Workforce Studies, AAMC, and IHS Markit Ltd; 2020. Dall T, Reynolds R, Chakrabarti R, Chylak D, Jones K, Iacobucci W. The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. Washington, DC: Center for Workforce Studies, AAMC, and IHS Markit Ltd; 2021.

